Radiotherapy
Cancer Treatment Options
Radiotherapy is a cancer treatment that uses ionizing radiation to control or destroy malignant cells in patients. In tumor treatment, high-energy radiation can kill or damage tumor cells and prevent them from continuing to grow, divide, or spread. Radiotherapy is a form of local treatment that typically only affects the area of the body being irradiated. It can cure some cancers that exist only in specific parts of the body. The effectiveness of radiotherapy is closely related to the precision of the equipment used. In recent years, radiation planning and precision in Hong Kong have significantly improved, resulting in a significant reduction in damage and side effects to surrounding healthy cells. Radiotherapy is suitable for treating breast cancer, head and neck cancer, lung cancer, oesophageal cancer, colorectal cancer, and more. In addition to cancerous tumors, radiotherapy is also used for benign tumors and hyperthyroidism. For inquiries about the cost of radiotherapy, please contact reVIVE Oncology and Cancer Centre.
Cost of Radiotherapy
The cost of radiotherapy depends on the type of cancer and the type and frequency of radiotherapy. The cost of radiotherapy is conservatively estimated to range from $50,000 to $100,000 or more. Patients should consult with their insurance agent if it is necessary to cover the higher costs of chemotherapy or radiotherapy.
Radiotherapy can be as a stand-alone treatment or in conjunction with other treatments such as surgery, chemotherapy, targeted therapy, immunotherapy or hormone therapy. It can also be used as an adjunctive treatment, which the doctor may use to reduce the size of a larger tumor prior to surgery. This helps to increase the certainty of complete removal of the tumor during surgery. It may also be used to eradicate the remaining cancer cells around the tumor after the resection, reducing the risk of recurrence. When the tumor cannot be removed by surgery, the doctor may choose radiotherapy and/or chemotherapy. This is done to relieve symptoms and pain in terminally ill patients.

- Redness and Irritation of The Skin in The Treated Area
- Fatigue
- Nausea and vomiting
- Diarrhoea
- Hair Loss
- Headache
- Difficulty in Swallowing
- Stiff Joints and Cramping
- Soft Tissue Fibrosis
- Sexual Dysfunction
Cancers Applicable for Radiotherapy
- Mammary Cancer
- Colorectal (intestinal) Cancer
- Oesophageal Cancer
- Head and Neck Cancer
- Lung Cancer
- Prostate Cancer
- Brain Tumour
The followings are the common side effects of radiotherapy:

- Protect the skin in the treatment area, avoid sunlight and wear loose clothing.
- Get enough rest and sleep.
- Eat small meals and avoid fried, spicy, sweet, and oily foods.
- Wear a suitable wig, headgear, or hat.
- Steroids or painkillers that lowered brain pressure can be taken to alleviate headaches.
- Appropriate exercise and massage can improve joint stiffness and cramping.
Post-electrotherapy Care

The effectiveness of radiotherapy is highly dependent on the precision with which it is administered, as it is necessary to kill cancer cells while minimizing the impact on normal cells. Our centre has the most advanced radiotherapy equipment available. The followings are some examples:
VMAT is a form of volumetric and rotational intensity-modulated radiation therapy. When the linear accelerator rotates 360, doctors will optimize precise control of the speed, radiation dose rate, and multileaf collimator through image guidance, and use a precise computer-based calculation system to concentrate the dose as much as possible in the tumor area while sparing normal tissue, improving treatment efficacy, and reducing side effects. This therapy is currently recognized as an effective treatment for various cancers, including tumors in the brain, head and neck, prostate, and cervix.
Compared to conventional treatments, VMAT significantly reduces treatment time by 50-80%, which effectively shortens the time patients with unstable conditions (such as unstable breathing) spend in the treatment room and reduces the risk of sudden emergencies.
Active Breathing Coordinator™
As breathing can move the tumor, the Active Breathing Coordinator can help patients hold their breath at the same lung volume consistently when undergoing simulation and radiation therapy. This minimizes body movement, improves radiation accuracy, and greatly reduces the radiation dose to the important organs or normal cells surrounding the tumor.
The Active Breathing Coordinator has a strict standard procedure throughout the entire treatment process. Before performing active breathing control radiotherapy, the medical team first customizes a mouthpiece for the patient to connect with the breathing control device, performs computed tomography (CT) simulation, designs a treatment plan and calculates radiation dose. After the doctor confirms the treatment plan, precise active breathing control radiotherapy will be conducted with the breathing coordinator.
Adaptive Radiotherapy
During a course of radiotherapy, patients may experience weight loss due to the loss of appetite, which can cause changes in their body shape and contour.
Adaptive radiotherapy can record the patient's contour, and help doctors formulate appropriate treatment plans through CT verification scans. The clear image quality allows doctors to observe the patient's daily condition and quantitatively measure the tumor response during radiotherapy, thereby enabling plan adaptation according to tumor changes.
Tomotherapy
Tomotherapy is an advanced therapy system that combines treatment planning, positioning and intensity-modulated radiation therapy (IMRT). It can accurately distinguish the site requiring radiation therapy, calculate the optimal beam distribution and dose, track changes in tumor shape and position, and concentrate the beam at the tumor to minimize damage to surrounding tissues and side effects.
Volumetric Modulated Arc Therapy
(VMAT)
Precisely combats cancer cells
In general, when the tumor has spread to a large area and is dispersed, radiotherapy is not recommended in order to avoid excessive side effects.
However, tomotherapy utilizes 360 incident angles of photon beams and synchronous movement of the treatment couch, and designs up to 51 angles of Helical Intensity-Modulated Radiation Therapy (IMRT) to accurately distinguish the site requiring radiation therapy, avoid normal tissues, and focus the beams on attacking cancer cells. In addition, with a 3D computer-assisted treatment planning system, CT-based adaptive image-guided radiotherapy (IGRT) system, precise patient positioning system, and quality assurance system, these technologies form a complete treatment system and provide patients with an efficient and safe treatment option.
For patients with multiple tumors throughout the body or requiring large-scale radiation, as tomotherapy can cover a range of up to 160 cm, it can reduce the treatment time to a single session.
Accurately locates the tissues
The patient’s posture during each treatment session can hardly be the same, and the location of the tumor and organs can vary every day. Therefore, it is necessary to take an image of the tissues with the built-in CT scanner prior to each treatment session and compare it with previous images to obtain a three-dimensional view of the changes and make adjustments immediately, facilitating precise treatment targeting the tumor.
Although this process takes one to four times longer than conventional treatment, it can help understand the changes in the tumor size and record the accumulated dose targeted to the tumor and surrounding tissues to personalize dose adjustments. By accurately calculating the dose distribution and tissue location, the therapy can protect normal tissues and avoid unnecessary side effects.
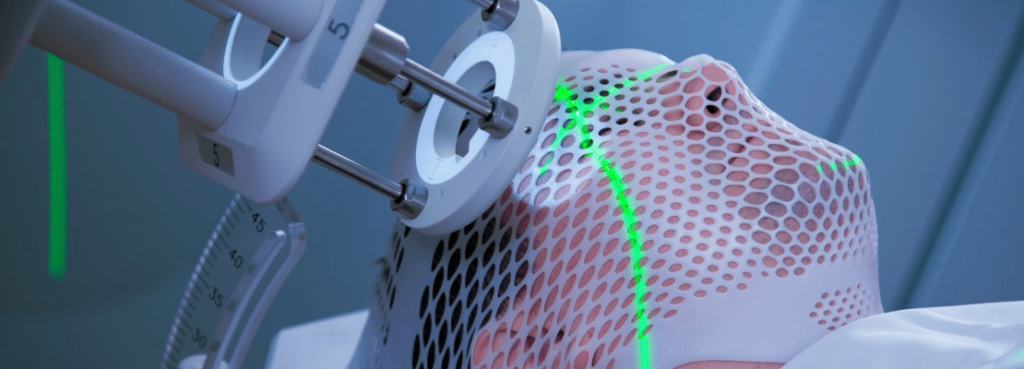
Stereotactic radiotherapy
Stereotactic radiotherapy is very precisely targeted radiation therapy that uses special tools to fix the patient’s position and ensure accurate radiation, thereby reducing damage to surrounding tissues. It is mainly used to treat tumors in the head and neck.
Stereotactic radiosurgery (SRS) uses high doses to completely destroy tumors in a few treatment sessions, requiring less time when compared to traditional low-dose radiotherapy. It provides a safe and effective treatment option for patients who are too old or too ill for surgery.
To make precise adjustments prior to stereotactic radiotherapy, doctors will utilize tomotherapy to observe real-time images of the patient's body and identify the exact location of the tumor. Tomotherapy can handle multiple tumor locations at once, which saves a lot of time. In addition, using Radionics' immobilization device can help target the tumor and minimize the impact on normal tissues.
Image-Guided Intensity Modulation Radiation Therapy
Intensity Modulation Radiation Therapy
Intensity Modulation Radiation Therapy (IMRT) emits high doses of tiny radiation beams to the body from different angles to intersect on the tumor while minimizing damage to surrounding normal tissues. IMRT can adjust the distribution of radiation doses based on the tumor's shape and surrounding tissue's location.
Image-Guided Technology
Image-guided technology improves the accuracy of radiation treatments. The patient’s posture during each treatment session can hardly be the same, and the location of the tumor and organs can vary every day. Therefore, it is necessary to take orthogonal X-ray images and CT scans prior to each treatment and compare them to the planning CT images. The patient’s position can be adjusted accordingly to ensure that the radiation is accurately directed as planned.
Three-Dimensional Conformal Radiation Therapy (3DCRT)
3DCRT involves studying the data of CT scans in a computer program, designing radiation beams that match the shape of the tumor and evenly distributing the beams from different angles. However, 3DCRT still has some room for improvement. Some tumors have a concave or “C” shape, for example, nasopharyngeal tumors often wrap around the cervical spine, which hinders treatment due to the concern of the spinal cord receiving excessive radiation. Normal tissues like the parotid glands may also receive high doses of radiation, leading to inevitable side effects. IMRT is an advanced type of 3DCRT that aims at controlling the intensity of radiation in the most appropriate way by using more sophisticated software to create treatment plans tailored for each patient.
How IMRT Works
During treatment planning, apart from visualizing the tumor and the surrounding region, it is also necessary to enter parameters such as the upper limit of doses. The computer planning program will calculate the parameters and develop an optimal plan which will be assessed by an oncologist. This process is called "inverse treatment planning". Tumors and other tissues can be divided into multiple small units, and the dose received by each unit is composed of a combination of tiny radiation beams from multiple incident angles.
As for the hardware, the tiny leaves of multi-leaf collimators can be arranged in different shapes as needed. Radiation beams were uniform and flat in the past, but now they can be shaped to non-flat beam profiles according to the treatment requirements. With dynamic multi-leaf collimators and dose adjustment technology, IMRT can achieve an ideal dose distribution and deliver optimal treatment outcomes for patients.
Superficial Radiation Therapy
Superficial radiation therapy can effectively treat skin cancer including basal cell carcinoma, squamous cell carcinoma and Kaposi's sarcoma.
The therapy uses low-energy X-ray beams within the range of 50-150 kV. The beam energy will only penetrate the skin surface and spare the deeper tissues, thus reducing scarring. The treatment can also prevent difficulties of reconstruction and the risk of disfiguring caused by surgical excision. For cases with a high risk of recurrence after surgery, adjuvant superficial radiation therapy can further improve the cure rate.
Prone Breast Radiation Therapy
In traditional breast cancer treatment, patients would receive treatment in a supine position. However, the current prone breast radiation therapy allows patients to lay in the prone position with the breast that requires treatment hanging away from the chest wall, reducing radiation exposure to lung/heart tissue and other normal tissues during treatment.
The dose-volume histogram shows that the lung tissues of patients who receive prone treatment receive less radiation exposure than that of those who receive supine treatment. In addition, patients with larger breasts can benefit from higher therapeutic effects with prone treatment.
A study of 245 women with early-stage breast cancer found that most patients accepted the prone position during their breast radiation therapy, with only a few patients (about 4.9%) reporting chest wall or rib pain, and none of them requiring a mid-treatment break. This position ensures that the radiation is evenly distributed to each part of the breast, while the top and bottom do not receive too much radiation. The prone position can be regarded as a more effective posture for treating breast cancer.
Remote High Dose Rate (HDR) Afterloading Brachytherapy
This therapy utilizes a radiation source (Ir192) to deliver radiation dosage at a short distance to the surface of a tumor by interstitial or intracavitary application. A high radiation dose can be delivered directly to the tumor while minimizing damage to surrounding tissues and organs.
Suitable cases for Brachytherapy include:
- Cancers of the uterine cervix, uterine body and vagina
- Mammary Cancer近距離劑量提升
- Boost in nasopharyngeal carcinoma treatment
- Recurrence and retreatment of neck cancer
- Intraluminal boost in oesophagal cancer treatment, etc.



